When Movement Isn't Easy: Living With Whole-Body Apraxia
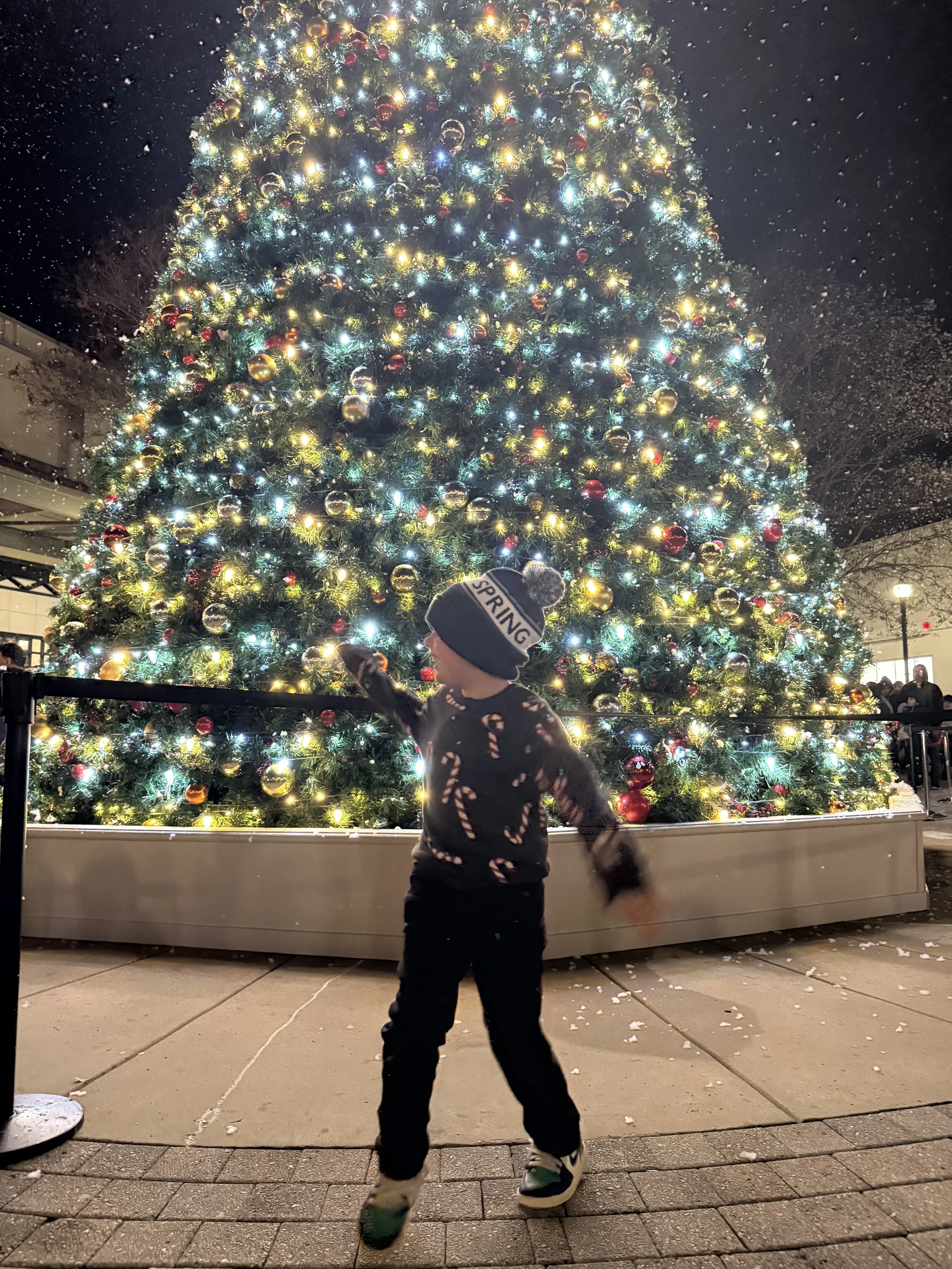
Last night at the ice skating rink, every skating walker was already rented. So there we were—one wall, two parents, one child who picked it up right away, and one very determined kid, and me calling out, “strong like a Christmas tree!” which is hilarious because the rest of the time we’re teaching them “flexible like a palm tree.”
There are parts of our story I’ve always struggled to explain, because they’re often invisible until they’re not.
Whole-body apraxia is one of those things.
Most people think apraxia is “just clumsiness.” Apraxia is what happens when the brain and body communicate differently, not incorrectly, not badly, just differently; and the timing doesn’t always line up.
Even as a seasoned nurse, I only really understood that by living it with my own child.
The Early Years: When Gravity Felt Personal
Back in the wobbly toddler days—the “tabby stage” , he would fall constantly.
Not trip.
Not stumble.
Just drop.
And he’d pop right back up every single time.
When he became a toddler, the falls didn’t stop. They just got bigger. We were going through ice packs like we ran a small clinic.
When we finally started Early Intervention ( that’s a story for a different day) his OT introduced a compression tank top.
We called it the “hug shirt.”
And suddenly, he looked more grounded. More connected. More aware of where he was in space. Not because he changed, but because his body finally got what it needed.
That’s when I realized this “little speech delay” + clumsiness combo was much more than met the eye.
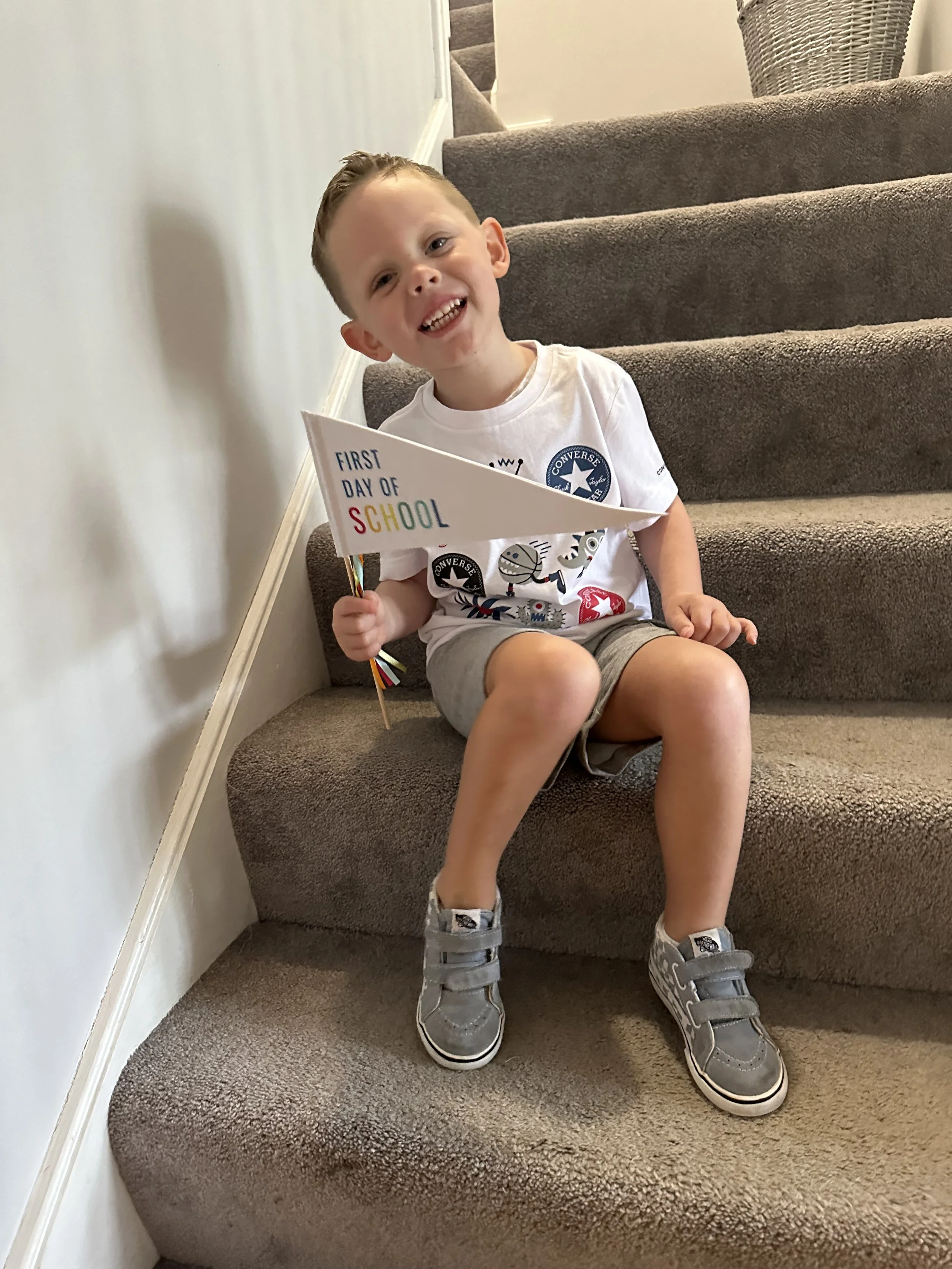
When He Started Advocating for Himself
About nine months later, right around the same time his formal diagnoses came in—he asked to stop wearing the hug shirt.
And within days, the falls returned. I filled out boo-boo report after report each day at preschool pickup.
Finding His Rhythm, Layer by Layer
At OT, they focused on primitive reflex work and sensory regulation. After years of advocacy, both his SLP and pediatric dentist signed off on the tongue-tie release at 4.5, and it made a bigger difference than anyone expected.
Then last winter on whim (aka me researching that they have neurodiversity classes) I signed them up for Taekwondo. It isn’t easy for him, but he loves it — I love how it works on core stability, confidence, sequencing, and is repetitive by nature.
His brain and body aren’t always in the same gear.
Sometimes his brain zooms ahead while his body lags behind. Other times his body moves fast and instinctively while his brain is still processing.
And with every layer of support and accommodation, the apraxia became less noticeable in familiar routines—not because we wanted to change him, but because we wanted him safe in his own body. His brain mapped the patterns. Built the pathways. Found its rhythm, that is until he tries something new.
That’s when we remember: the apraxia never left. He’s just built a bigger toolkit to explore more of the world.
Enter Ice Skating
Which brings us back to the rink. Ice skating is a whole new motor plan his brain had never mapped before.
We arrived ready for a fun night—tummies filled with chocolate chip pancakes and milk, snow* fluttering in the sky, a perfectly lit rink… with every skating walker already rented (of course!).
So we improvised.
We divided and conquered.
We switched when that didn’t work.
We left after an honest go of it—with promises to return when we can use the walker.
What Whole-Body Apraxia is
Apraxia is when the brain’s plan and the body’s timing don’t always line up.
It can impact: balance, spatial awareness, core stability, rhythm, motor planning, crossing midline, sequencing, eye coordination
This is why so many kids get mislabeled as “careless,” “clumsy,” “disruptive,” or “unfocused.”
They’re NONE of those things.
They’re navigating a motor system that needs information delivered differently. And I promise you, they’re already trying their hardest.
When to Seek Professional Input
If you’re noticing patterns like:
frequent falls past age 3
difficulty with motor tasks peers have mastered
struggles with sequencing or coordination
challenges with new movement patterns
As always, Trust your instincts.
An occupational therapy evaluation can provide clarity and open doors to support—whether through therapy, at-home activities, or simply understanding your child’s sensory needs.
Thank you for being here, for learning, for listening, and for honoring the way your child moves through the world.
Next time I’ll be sharing how apraxia affects reading and pre-reading skills.
If this post helped you feel seen, share it with a parent who needs the language for what they’re noticing too.
~ Christie
Behind the Stims | Stims & Smiles